By Sarah Ladd
Kentucky Lantern
Fewer Kentuckians have health insurance through kynect after subsidies that helped millions of Americans afford health insurance expired late last year but the decline is not as drastic as advocates had feared.
Overall, about 89,000 Kentuckians enrolled in an Affordable Care Act health plan for 2026, down from about 97,000 last year, according to Priscilla Easterling, the director of outreach and enrollment at Kentucky Voices for Health.

“We saw a drop, but not nearly as significant as we thought it might be,” she said.
Not all who decided to go uninsured were young and healthy, Easterling said: “It runs the gamut.”
“It tends to be younger, healthier folks who are foregoing health insurance,” she said. “But … I’ve genuinely worked with folks well into their 60s who are also having that conversation about foregoing health insurance and just kind of either relying on the federally qualified health centers in their area, rationing medicine or just not going to the doctor at all.”
Nearly 11,000 Kentuckians cancelled their plan for 2026, she said, but 14,000 new patients enrolled for the first time.
“Even with those enhanced premium tax credits expiring, we still saw more people come into Kynect for the first time than left it, which I still think is a great thing,” Easterling said.
Still, she worries about the coming months, when Kentuckians could face economic changes they couldn’t foresee.
“Folks’ budgets change all the time, and health insurance is often the first thing that they drop,” she said. “And so I’m very concerned that we’re going to see a lot more of that this year than, maybe, than in previous years.”
A ‘very tough position’
The U.S. House voted in January to extend the subsidies, which expired Dec. 31. The Senate, however, has not yet voted on the measure.
This “will-they, won’t-they?” limbo leaves Kentucky in a “very tough position,” said Easterling.
ACA premiums have increased by more than 20%, the Commonwealth Fund reported in January, “in large part because insurers believe they are facing increased risk due to the expiration of enhanced premium tax credits and other policies.” The Commonwealth Fund also reported that the insured population is likely to include fewer healthy people, which increases the risks facing the insurance companies.

Around 16,000 Kentuckians switched their health plan to one with a lower monthly premium but higher deductible (shifting from gold or silver plans to bronze, for example), said Easterling, who also helps Kentuckians navigate the health insurance marketplace as a kynector.
“That speaks to that price difference: What can folks afford?” said Easterling. “And those silver and gold plans, for a lot of folks, were just out of reach.”
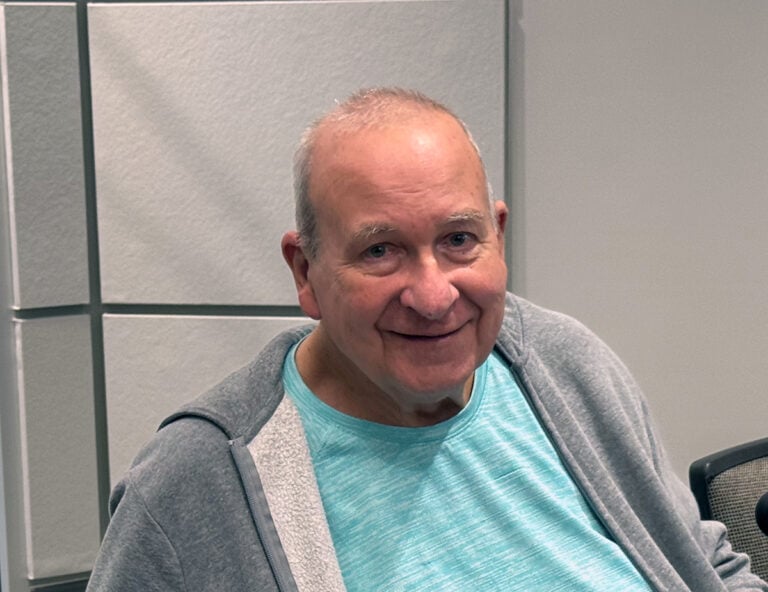
This was true for Kenton County’s David Roode, who switched from a silver plan to a bronze.
Last November, Roode logged into his account and saw he and his wife’s health plan, which had been $150, was increasing to $450 a month.
“I had this initial sticker shock of, like, ‘I don’t want to look at this, oh my gosh,’” he recalled. “And so, I just logged out.”
Roode and his wife are both musicians (he’s a trombonist and she is a pianist) who work in performance and orchestras in a freelance capacity, which means “I don’t get health insurance through any one place,” he said.
They considered several options in response to the insurance cost hike, including getting a more expensive plan with a lower deductible and finding extra employment to pay for it. Eventually, they chose a bronze plan with a similar monthly cost to their 2025 plan, but with a higher copay and higher deductible.
“The most scary downside is that the deductible is … around maybe $10,000 or something. So, it’s a hefty deductible,” he said. “Fingers crossed that we don’t need to go into that this year. All of our medical usage has been mainly preventative stuff.”

Roode and his wife don’t have a dedicated emergency health savings account big enough to cover the $10,000 deductible if faced with a medical crisis, he said.
“We could manage it,” he said, but: “It would be a pretty hefty financial blow. So, I would not want that to happen.”
Rachel Eppley, who is from Laurel County and lives in Lexington, works as a church administrator. Her husband, a former teacher, left education to focus on therapy, his passion, in 2024.
“It was a shocking change for us — figuring out ‘how do we get insurance by ourselves?,” she said. They turned to the marketplace, which was initially frustrating — they enrolled in a plan they thought was similar to what they’d had before, but none of their providers were in network.
When the subsidies expired, their plan was going to increase from around $550 to $1,300, Eppley said. To have a wider selection of providers, they would have owed around $1,800 per month on a plan for themselves and their two children.
They eventually settled on a plan for about $800 per month. For the foreseeable future, neither of them are interested or able to change jobs or careers to less fulfilling work that offers health care coverage.
“People should have the freedom to … have (jobs) that they love,” she said, “without having to sacrifice health insurance.”
The ‘equation at play’ for children

Terry Brooks, the executive director of Kentucky Youth Advocates, said having higher health care premiums “is a certainty with negative consequences” for children in the state.
In 2023, about 97% of Kentucky children had health insurance, which is an indicator of access to preventive services and overall health and wellbeing.
“We know the high — and common sense — equation at play is that, if parents are covered, kids get coverage. And the inverse is true as well. A parent not covered by health insurance is less likely to ensure that son or daughter has coverage,” Brooks said. “Observers of all political stripes acknowledge that recent federal changes will most likely result in fewer adults being covered. And if history is a guide, then we are going to see a decline — at least in the longer term — of kid coverage as well.”
A complicated — but possible — editing process
If Congress extends the subsidies, Easterling said, Kentucky can recalculate plans and adjust the costs. This would be “a very complicated process” for the state, she said, and also depends on what that extension looked like.
If the credits were extended the full three years that the U.S. House aimed for, Kentucky would likely open a brief special enrollment window so people could shop for plans again, Easterling explained.
Meanwhile, the “more immediate risk to Kentucky’s kids is a kitchen table economics issue,” said Brooks with Kentucky Youth Advocates.
“Higher premiums will result in less money on that table for families. And economic stress points will inevitably reveal themselves in food insecurity, housing instability and family disruptions,” Brooks said. “The federal changes, in other words, will almost certainly affect kids in a number of ways — all on the negative — in both the long-term and the immediate.”
Kentucky Lantern is part of States Newsroom, a nonprofit news network supported by grants and a coalition of donors as a 501c(3) public charity. Kentucky Lantern maintains editorial independence. Contact Editor Jamie Lucke for questions: info@kentuckylantern.com.