By Tom Latek
Kentucky Today
Cabinet for Health and Family Services officials on Tuesday updated a legislative committee on the new waiver issued by the federal Centers for Medicare and Medicaid Services last week.
CMS once again approved the state’s Section 1115 Medicaid waiver known as Kentucky HEALTH, an acronym for Helping to Engage and Achieve Long Term Health, which includes a community engagement requirement for eligibility.
A federal judge had halted implementation of the waiver program on June 29, 2018, just two days before Kentucky Health was to begin.
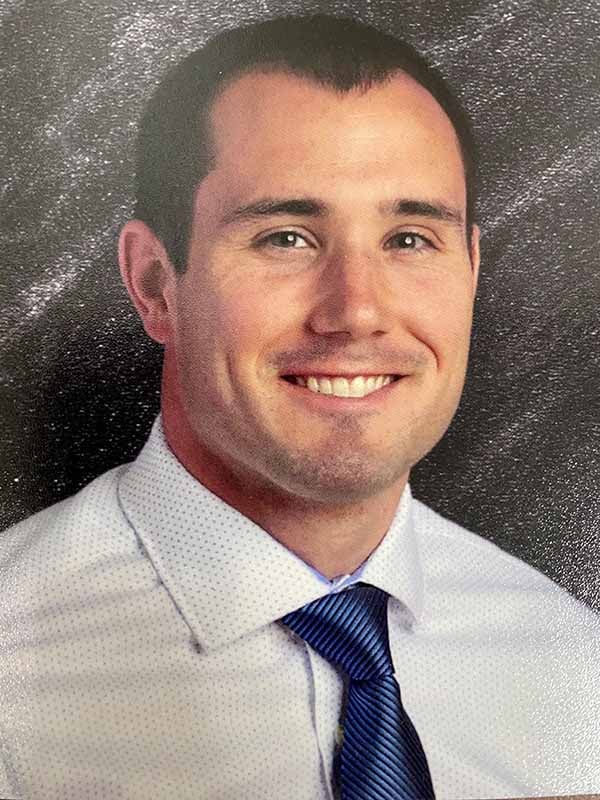
CHFS Secretary Adam Meier told the Interim Joint Health and Welfare and Family Services Committee that very little has changed from the original waiver.

“There were some updates to the monitoring and evaluation plan requirements to bring them more in line with what they have in other states.”
Meier said they also asked CMS to find a way to treat domestic or other personal violence victims as part of the medically frail category, which would exempt them from the community engagement requirement. “That was something CMS was able to accomplish with the re-approval.”
Kentucky HEALTH would put about 460,000 “able-bodied” adults in a plan with limited benefits that didn’t include dental and vision. However, individuals could earn points toward paying for dental and vision care through volunteer activities in the community or by taking online classes through a “My Rewards” system.
The newly approved program can begin as soon April 1, 2019. Accordingly, the PATH, or Partnering to Advance Training and Health, community engagement component will be rolled out regionally over a several month period, beginning no sooner than April 1, 2019.
There have been reports that up to 95,000 people would lose coverage because of the Medicaid waiver, and Rep. George Brown, D-Lexington, asked if that was the case.
“I don’t have a crystal ball as to how many will lose coverage,” Meier said. “But what we can say is we have worked with CMS very diligently to ensure that any appropriate exemptions are included, so we can protect any adverse consequences of waiver policies that would be unintended.”
Meier said a large part of negotiations with CMS “was to find ways to mitigate any unnecessary interference with people’s ability to have access to care. The same people that have access today, will have access post-implementation. We have provided the right kind of exemptions and exceptions.”
Brown responded to Meier’s comments saying, “Coverage of citizens in the Commonwealth should not be based on the bottom line for hospitals and doctors, coverage of citizens in the Commonwealth should be most important.”
Rep. Melinda Gibbons Prunty, R-Belton, asked Meier if the courts could stop the waiver again.
“There’s always a chance, but CMS went back and did a more thorough review,” Meier said.
“I think they’ve done a really good job of drawing out the things we did in the process that were maybe missed in the judicial review the first time around, so we can better highlight all the considerations and the thought that went into ensuring this program is designed to engage people, but not create issues with people ha