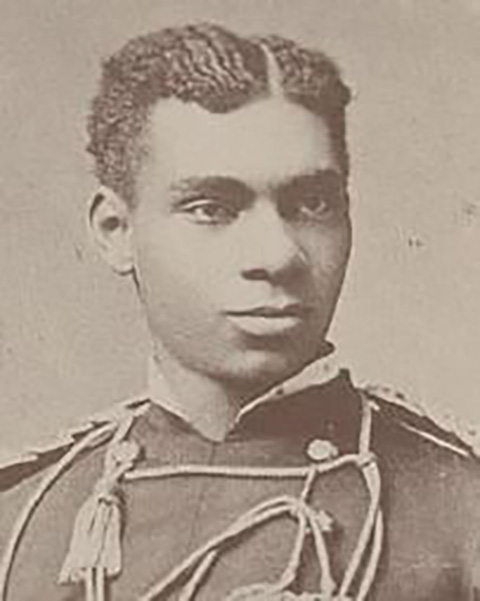
In Covington, after 26 years of service, Assistant Chief Chip Terry went into a deep depression shortly after retirement. Everybody I have talked to who knew him has told me that he was a wonderful family man who loved his community and his children. But his service to the community took a toll on his life and in September 2017 he took his own life.
In a speech that recapped his life at his retirement, while addressing the city leaders he said, “Most people don’t realize the horrific and haunting tragedies that firefighters see. Nor do they comprehend the psychological impact. “People don’t see at three in the morning when a young lieutenant has to put two toddlers and their grandmother in a body bag (or) a 16-year-old boy hangs himself with an electrical cord,” Terry told the city commission. “How do you close your eyes at night after you make that run? I’ve seen people shoot themselves in the head. I’ve seen children beaten and burned. Today I can lay down in bed and close my eyes and still see the faces of those toddlers.”

It was later determined that Terry struggled with post-traumatic stress disorder (PTSD) and it overwhelmed him.
Being a first responder subjects individuals to traumatic events, resulting in a higher risk of
developing PTSD, major depressive disorder (MDD), panic disorder (PD), and generalized anxiety disorder (GAD).
Exposure to multiple traumatic stressors could also exacerbate other pre-existing conditions. The presence of any mental health disorders in these individuals can also be associated with diminished ability to work efficiently, early retirement, substance abuse, and suicide.
In my line of work, it’s easy for me to identify those workers compensation injuries where people have physical injuries from strain, broken bones, contusions, and lacerations, but how do you detect PTSD injury? More importantly, how do you prevent it?
I won’t dare say this is above my pay grade, because it’s still my job to identify and prevent “all” injuries/illnesses and the first step is to increase the awareness of PTSD.
Last week I identified the risk and the causes for this illness amongst our first responders, and this week I want to help address ways to prevent it.
What I do know is that much more needs to be done to identify, treat, reduce and prevent PTSD with first responders. For instance, although so many first responders are being treated for PTSD nationwide, OSHA has yet to adequately address this exposure. Our medical community is well aware of this illness, so why hasn’t OSHA gotten on board to marshal their efforts to help identify, prevent and enforce changes?

OSHA’s mission is to ensure safe and healthful working conditions for working men and women by setting and enforcing standards and by providing training, outreach, education, and assistance. Their motto is to require employers to implement an Injury and Illness Prevention Program tailored to the actual hazards in their workplaces.
While OSHA has done a good job of preventing other workplace illnesses, what is OSHA doing to prevent PSTD illness in the workplace for first responders?
OSHA identifies PTSD as a mental illness which is usually not a recordable accident, but they do make an exception to PTSD claims and do classify them as a recordable accident. But that is about as far as they go. There isn’t a written standard in their CFR 1910 or 1926 guidelines to help identify, guide, train, education or assistance employers to reduce and prevent such illnesses.
The Ruderman White Paper on Mental Health and Suicide of First Responders Foundation revealed that first responders (policemen and firefighters) are more likely to die by suicide than in the line of duty. In 2017, there were at least 103 firefighter suicides and 140 police officer suicides, and those numbers don’t include all the suicides from retired first responders. But you won’t see any of these suicides listed as a workplace fatality. Didn’t this illness develop due to the exposures within their work environment?
Because it’s viewed more as a mental illness, we don’t see OSHA studies, reports or committee’s working diligently to try to prevent them.
The National Institute Occupational Safety and Health (NIOSH) whose mission is “to develop new knowledge in the field of occupational safety and health and to transfer that knowledge into practice” and they offer nothing for PTSD for first responders on their website.
The Center for Disease and Control (CDC) acknowledged in a publication that “there is a substantial literature that has examined the risk factors, symptom presentation, course, and comorbidities of PTSD in this population. However, to our knowledge, there are no systematic reviews of treatment studies for first responders.”
It’s time for our governmental agencies to come together to try to drive the number of these suicides down. When people were dying from respiratory illnesses related to asbestos exposure, even after these workers were well into their retirement, all these governmental agencies jumped into action and created an entirely new standard and forced employers to comply.
The good thing is PTSD is a compensable injury when it comes to workers compensation and the medical community fully supports treating it if someone is seeking help. The hurdle is that many first responders think that seeking help will be perceived as “weak.” There is also the stigma surrounding mental health issues, which stereotypes those with mental health problems as being defective or weaker. This sometimes leads to prejudice and discrimination in the workplace.
As a result, first responders fear that any admission to PTSD will force them to out of their profession, which is hard to envision because many view their work as their identity.
Education can go a long way and we should better educate and train both management and employees in areas such as anti-stigma and general awareness, resiliency, signs, and symptoms, how to seek support, and how to support others who may be suffering from PTSD.

All new hires should be educated on the causations of PTSD and how to recognize the systems. The message should consistently be “It’s OK to be OK — and it’s OK to be not OK.”
Consistent mental health education on understanding, monitoring, dealing with, and preventing PTSD is vital in keeping employees informed, prepared, and listening. Employees must fundamentally understand what PTSD and a mental health disorder truly are and how they can impact an individual. Education and training must include monitoring behavioral changes that are viewed from a chronological standpoint.
The change in mental attitude and perception of mental health issues must start from the leadership at the top since first responder workplaces have very strict hierarchies. The complex relationship between PTSD, traumatic situations and why disorders manifest has to be explained and understood.
Here are some other ways supervisors can help:
· Understand that being angry or withdrawn are signs of PTSD.
· Encourage the person to speak to someone trustworthy for help.
· Ask how you can support the worker – even if he or she doesn’t want to talk about it.
· Provide access to support services – as well as time away to attend services – and be understanding to workers returning to work after an incident.
As for the rest of us, we should all take the time to stop and thank a first responder for their commitment to serving us and our community.
A simple act of generosity can go a long way when dealing with a first responder. Your respect and kindness in a small way may make up for that next jerk that they will later encounter or help take their minds off that emotional scar that they are dealing with.
Be Safe My Friends

Keven Moore works in risk management services. He has a bachelor’s degree from the University of Kentucky, a master’s from Eastern Kentucky University and 25-plus years of experience in the safety and insurance profession. He is also an expert witness. He lives in Lexington with his family and works out of both Lexington and Northern Kentucky. Keven can be reached at kmoore@roeding.com.